Root canal treatment is designed to save your tooth and eliminate infection, but sometimes complications can arise. One of the most concerning issues patients face is developing a gum infection after root canal treatment. While this situation can feel alarming, understanding why it happens, recognizing the symptoms early, and knowing your treatment options can help you navigate this challenge with confidence.
If you’ve recently undergone a root canal and notice unusual changes in your gums, you’re not alone. Thousands of patients experience post-treatment complications each year, and most can be successfully resolved with prompt professional care. This comprehensive guide will walk you through everything you need to know about gum infections following root canal procedures, from identifying warning signs to understanding prevention strategies.
Understanding Root Canal Treatment and Potential Complications
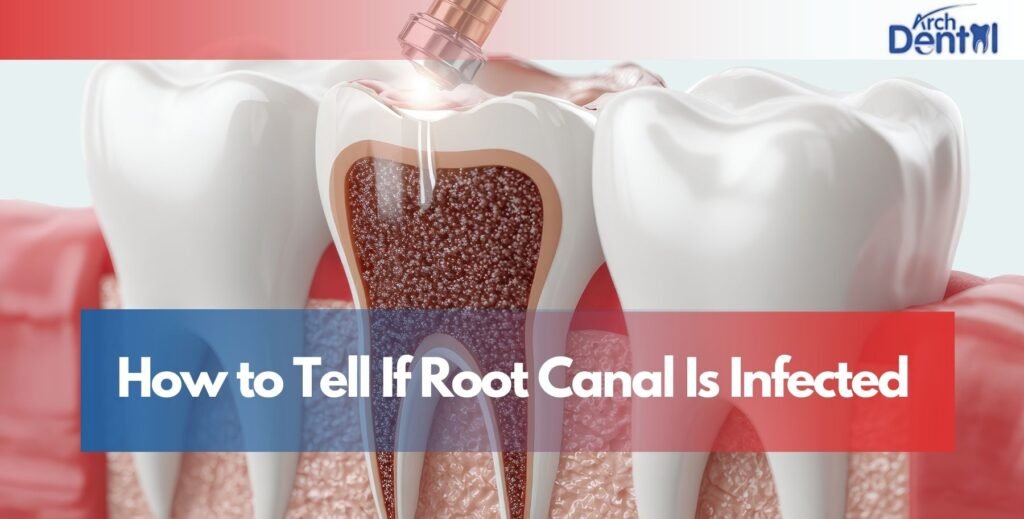
Root canal therapy involves removing infected or damaged pulp tissue from inside your tooth, cleaning the root canals, and sealing them to prevent future bacterial invasion. The procedure boasts a success rate of approximately 85-97%, making it one of the most reliable treatments in dentistry. However, like any medical procedure, complications can occasionally occur.
Post-root canal infection can develop for several reasons: incomplete removal of bacteria, contamination during the procedure, inadequate sealing of the canals, or delayed placement of a permanent restoration. Sometimes, complex root anatomy makes it challenging to access and clean every canal completely. Additionally, if bacteria find their way into the treated area through a compromised temporary filling or cracked tooth structure, infection can take hold in the surrounding gum tissue.
Your gums play a crucial role in supporting your teeth and protecting underlying bone structure. When bacteria invade gum tissue near a recently treated tooth, inflammation and infection can compromise healing and threaten the success of your root canal. Understanding this connection helps explain why maintaining excellent oral hygiene after your procedure is absolutely essential.
The risk of dental infection after endodontic treatment increases when patients have compromised immune systems, pre-existing periodontal disease, or fail to follow post-treatment care instructions. Your dentist’s skill and adherence to sterile techniques during the procedure also significantly impact infection risk.
Common Causes of Gum Infection Following Root Canal
Understanding why gum infections develop after root canal treatment helps you take preventive measures and recognize risk factors that may compromise your healing process.
Incomplete Bacterial Removal
Despite advanced techniques and equipment, some bacteria may survive the root canal cleaning process, particularly in teeth with complex or curved canals. These persistent bacteria can multiply and spread to surrounding gum tissue, causing infected gums after root canal symptoms. Anatomical variations like accessory canals or calcified structures can harbor bacteria that standard cleaning procedures might miss.
Compromised Temporary Filling
The temporary filling placed after your root canal serves as a critical barrier against bacterial invasion. If this filling becomes loose, cracks, or falls out before your permanent restoration is placed, bacteria from your mouth can enter the treated tooth. This contamination often leads to gum swelling after root canal and subsequent infection in the surrounding soft tissues.
Vertical Root Fractures
Sometimes the tooth structure itself develops microscopic cracks during treatment or afterward due to biting forces. These fractures create pathways for bacteria to reach areas that were previously sealed, resulting in root canal complications including gum infection. Vertical root fractures are particularly problematic because they’re difficult to detect and often require tooth extraction.
Pre-existing Periodontal Disease
If you had undiagnosed or untreated gum disease before root canal, the bacteria associated with periodontal infection can complicate your recovery. These bacteria may take advantage of the trauma and inflammation from your root canal procedure to establish a more aggressive infection in the already compromised gum tissue.
Delayed Crown Placement
When too much time passes between your root canal treatment and placement of a permanent crown, the tooth becomes vulnerable. The temporary restoration may deteriorate, and the tooth structure itself can weaken, both increasing the risk of bacterial contamination and abscess after root canal treatment.
Recognizing Symptoms of Infected Gums After Root Canal
Early detection of infection symptoms allows for prompt treatment, preventing complications and ensuring the long-term success of your root canal procedure and overall oral health.
Persistent Swelling and Redness
One of the earliest signs of gum inflammation after root canal is visible swelling around the treated tooth. While mild swelling immediately after your procedure is normal, pronounced or worsening swelling that persists beyond three to five days indicates a problem. The affected gum tissue may appear bright red, shiny, and feel tender or painful when touched.
Unusual Drainage or Pus Formation
The presence of pus is an unmistakable indicator of active infection. You might notice yellowish, white, or greenish discharge seeping from your gums near the treated tooth. This periodontal infection after root canal often produces a foul taste and odor. Some patients observe a small pimple-like bump on their gum that intermittently drains fluid, temporarily relieving pressure.
Throbbing Pain That Worsens Over Time
While some discomfort after a root canal is expected, pain after root canal infection typically feels different from normal healing soreness. Infected gums produce a deep, throbbing pain that may intensify when you lie down or apply pressure to the area. This pain often doesn’t respond well to over-the-counter pain relievers and may disrupt your sleep.
Elevated Temperature and Systemic Symptoms
A low-grade fever in the first 24-48 hours after your root canal can be normal, but a persistent or high fever signals systemic infection. You might experience chills, general malaise, or fatigue as your body fights the bacterial invasion. These signs of infection after endodontic therapy indicate the problem may be spreading beyond the localized area.
Changes in Gum Texture and Bleeding
Infected gum tissue often feels softer or spongier than healthy tissue. You might notice increased bleeding when brushing or flossing near the affected tooth. The gums may appear to be pulling away from the tooth, creating pockets where bacteria can accumulate. These changes in gingival health post-root canal require professional evaluation.
Effective Treatment Options for Post-Root Canal Gum Infections
Modern dentistry offers multiple approaches to treating gum infections after root canal therapy, ranging from conservative antibiotic therapy to surgical interventions when necessary for resolution.
Antibiotic Therapy
When you develop bacterial infection after root canal, your dentist will likely prescribe antibiotics to combat the infection systemically. Common choices include amoxicillin, clindamycin, or metronidazole, depending on your medical history and the suspected bacteria involved. It’s crucial to complete the entire antibiotic course even if symptoms improve, as stopping early can lead to antibiotic-resistant bacteria.
Professional Cleaning and Drainage
If an abscess on gum after root canal has formed, your dentist may need to drain it to relieve pressure and remove infected material. This procedure involves making a small incision to allow pus to escape, followed by thorough cleaning of the area. Professional scaling and root planing may be necessary to remove bacterial deposits from the gum pockets surrounding the affected tooth.
Root Canal Retreatment
Sometimes the original root canal treatment requires revision to address persistent infection. Endodontic retreatment involves reopening the tooth, removing the previous filling material, and thoroughly cleaning and disinfecting the canals again. Your dentist will look for missed canals, cracks, or other issues that may have allowed bacteria to survive or re-enter the tooth.
Apicoectomy Surgery
When infection persists at the root tip despite retreatment, an apicoectomy after a failed root canal may be necessary. This surgical procedure involves accessing the root tip through your gum tissue, removing the infected portion of the root, and sealing it from the end. This approach can save teeth that would otherwise require extraction.
Tooth Extraction as a Last Resort
In cases where infection cannot be controlled or the tooth structure is too compromised to save, extraction becomes the most appropriate option. Following tooth removal due to root canal failure, your dentist will discuss replacement options such as dental implants, bridges, or partial dentures to restore function and appearance.
Prevention Strategies to Avoid Gum Infections
Taking proactive steps to maintain optimal oral hygiene and following your dentist’s post-treatment instructions significantly reduces your risk of developing painful and problematic gum infections.
Maintain Impeccable Oral Hygiene
The foundation of preventing infection after root canal lies in excellent oral hygiene. Brush gently but thoroughly twice daily using a soft-bristled toothbrush, paying special attention to the gum line around your treated tooth. Floss carefully once daily, and consider using an antimicrobial mouthwash to reduce bacterial load in your mouth.
Attend All Follow-Up Appointments
Never skip scheduled follow-up visits with your dentist. These appointments allow your dental professional to monitor healing, address concerns early, and ensure your temporary filling remains intact. Timely placement of your permanent crown is crucial for long-term root canal success and preventing bacterial contamination.
Avoid Hard or Sticky Foods
Protect your treated tooth by avoiding foods that could damage the temporary restoration or stress the tooth structure. Hard candies, ice, popcorn kernels, and sticky substances like caramel can compromise your temporary filling, creating entry points for bacteria. Chew on the opposite side of your mouth when possible during the healing period.
Address Underlying Periodontal Disease
If you have existing gum disease, work with your dentist to bring it under control before and after your root canal. Treating periodontal infection reduces the bacterial burden in your mouth and creates a healthier environment for healing. Regular professional cleanings become even more important when you’ve undergone endodontic treatment.
Follow Post-Treatment Instructions Carefully
Your dentist provides specific care instructions for a reason. Take prescribed medications as directed, manage discomfort appropriately, and contact your dental office if you notice any concerning symptoms. Being proactive about post-root canal care significantly reduces your risk of developing complications like gum infections.
Conclusion
Developing a gum infection after root canal treatment can be distressing, but it’s a manageable complication when addressed promptly. By recognizing warning signs like persistent swelling, drainage, unusual pain, or fever, you can seek treatment before the infection worsens or spreads. Remember that most infections respond well to appropriate intervention, whether that involves antibiotics, professional cleaning, retreatment, or surgical procedures.
Your oral health is an investment in your overall wellbeing, and staying vigilant after dental procedures protects that investment. Don’t hesitate to contact your dental provider if something doesn’t feel right during your recovery. Early intervention almost always leads to better outcomes. If you’re experiencing symptoms of infection or have concerns about your root canal healing process, the compassionate professionals at your trusted Dentist in Northampton, MA are ready to provide expert evaluation and personalized treatment to restore your comfort and oral health.
Frequently Asked Questions
Can a root canal cause ear pain?
Yes, ear pain after a root canal is relatively common due to shared nerve pathways. The trigeminal nerve serves both your teeth and ears, so inflammation from dental treatment can create referred pain in your ear. This typically resolves within a few days as healing progresses.
What to do if there is an infection after a root canal?
Contact your dentist immediately if you suspect infection. Don’t wait for symptoms to worsen. Your dentist will examine the area, possibly take X-rays, and prescribe antibiotics if needed. They may also drain any abscess and determine if retreatment is necessary.
How long does it take for gums to heal after a root canal?
Gum tissue typically heals within 7-10 days after a root canal, though complete internal healing of the tooth and surrounding bone can take several weeks to months. Minor tenderness and sensitivity during the first few days is normal and should gradually decrease.
Can a tooth infection cause diarrhea?
While rare, a severe spreading tooth infection can cause systemic symptoms including diarrhea as your body fights the bacterial invasion. More commonly, antibiotics prescribed to treat dental infections cause diarrhea by disrupting normal intestinal bacteria. Contact your doctor if diarrhea is severe or persistent.
What are signs a tooth infection is spreading?
Warning signs include high fever above 101°F, rapid facial or neck swelling, difficulty breathing or swallowing, severe fatigue, confusion, rapid heart rate, or feeling extremely ill. These symptoms indicate a potentially serious condition requiring immediate emergency medical attention.