Root Canal Treatment is one of the most effective procedures in modern dentistry for saving teeth that have been severely damaged by decay or infection. While this treatment boasts a high success rate of approximately 95%, there remains a small possibility that complications, including infection, can develop even after the procedure is completed. Understanding the warning signs of post-treatment infection is crucial for protecting your oral health and ensuring the long-term success of your root canal.
Many patients assume that once a root canal is finished, all potential problems are behind them. However, the days and weeks following treatment require vigilance and awareness of symptoms that might indicate complications. Recognizing these signs early and seeking prompt dental care can make the difference between a simple intervention and more extensive treatment. Whether you’re preparing for an upcoming root canal or have recently completed one, knowing what to watch for gives you the power to protect your investment in your dental health.
Understanding Root Canal Infections
An infection after root canal treatment occurs when bacteria invade the treated tooth or surrounding tissues despite the thorough cleaning and sealing performed during the procedure. While dentists take extensive measures to eliminate all bacteria from the tooth’s canal system during treatment, certain factors can allow infection to persist or develop afterward.
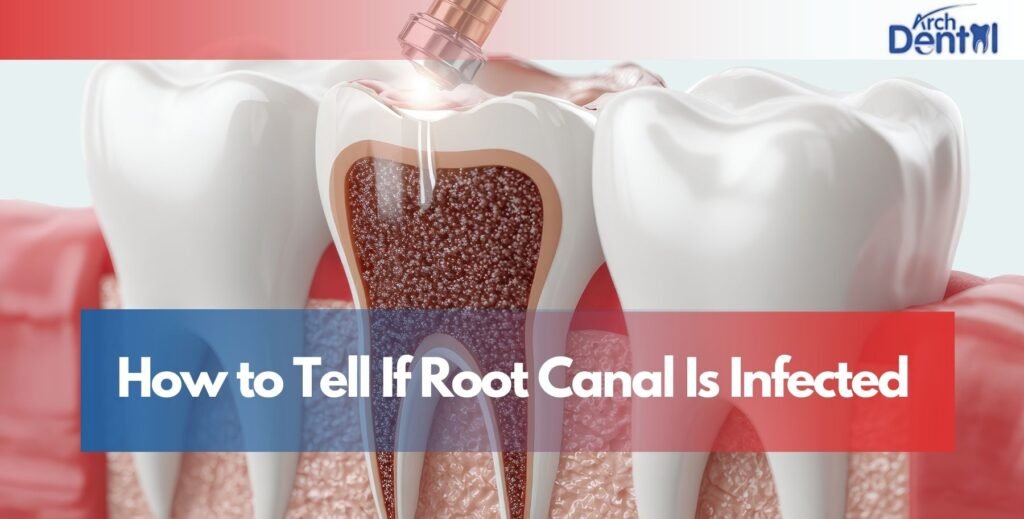
The root canal procedure involves removing infected or damaged pulp tissue from inside the tooth, thoroughly cleaning and disinfecting the canal system, and then sealing it with a rubber-like material called gutta-percha. A temporary or permanent filling is then placed to seal the access point. When performed correctly, this process eliminates the infection and prevents future bacterial invasion.
How Infections Develop After Treatment
Several mechanisms can lead to post-treatment infection. Sometimes, complex canal anatomy with tiny branches or unusual curves makes it difficult to reach and clean every area during the procedure. Bacteria hiding in these inaccessible spaces can survive and multiply after treatment.
A cracked or damaged tooth can provide pathways for bacteria to enter the sealed canal system. If the temporary filling becomes loose or falls out before the permanent restoration is placed, this creates an opening that allows bacteria to re-contaminate the cleaned canals. Additionally, if a permanent crown or filling isn’t placed promptly after root canal therapy, the tooth remains vulnerable to bacterial invasion.
In some cases, the sealing material may not completely fill the canal to the very tip of the root, leaving tiny voids where bacteria can accumulate. Occasionally, the infection may have already spread beyond the tooth into the surrounding bone before the root canal was performed, requiring additional treatment beyond the procedure itself.
Early Warning Signs of Infection
Recognizing the early signs of a tooth infection after root canal treatment allows for prompt intervention that can prevent more serious complications. While some discomfort immediately after the procedure is normal, certain symptoms warrant immediate attention from your dentist.
Persistent or Worsening Pain
It’s normal to experience some tenderness and sensitivity for a few days following root canal treatment as your body heals. However, pain that persists beyond a week, gradually intensifies rather than improving, or suddenly becomes severe after initially feeling better are all red flags that something may be wrong.
Pain from infection is typically described as throbbing, constant, and sometimes radiating to adjacent teeth, your jaw, or even your ear. Unlike the temporary discomfort of healing, infection-related pain often interferes with sleep and daily activities, and it doesn’t respond well to over-the-counter pain relievers.
Swelling and Inflammation
Mild swelling around the treated tooth for the first few days after treatment can be normal, but gum infection after root canal often manifests as swelling that develops several days after the procedure or doesn’t improve with time. The swelling may appear as puffiness in the gums around the tooth, visible swelling in your cheek or jaw area, or a noticeable bump or pimple-like formation on the gum near the treated tooth (called a fistula).
Swelling that feels warm to the touch, continues to expand, or is accompanied by redness indicates active infection requiring immediate professional attention. If swelling extends to your face, neck, or causes difficulty breathing or swallowing, this constitutes a dental emergency requiring immediate medical care.
Unusual Discharge or Bad Taste
The presence of pus or other discharge is a clear sign of infected root canal. This may appear as a yellowish or whitish fluid draining from the gum near the treated tooth, an unpleasant taste in your mouth that persists despite brushing, or visible pus when you gently press on the gum around the tooth.
A fistula—a small pimple-like bump on the gum—often drains pus intermittently, temporarily relieving pressure and pain before filling again. While this drainage may provide momentary relief, it indicates ongoing infection that requires treatment, not a problem that has resolved itself.
Recognizing Symptoms of Jaw Infection After Root Canal
Symptoms of jaw infection after root canal treatment are particularly concerning because they indicate that the infection has spread beyond the tooth into the surrounding bone and tissues. This represents a more serious complication that requires immediate professional attention to prevent further spread.
Pain and Tenderness in the Jaw
Jaw pain associated with infection differs from normal post-treatment discomfort. It presents as deep, aching pain in the jaw bone that may worsen when chewing or applying pressure, tenderness when touching the jaw or face near the treated tooth, or difficulty opening your mouth fully due to pain and muscle tension.
The pain may radiate along your jaw line or feel like it’s affecting multiple teeth rather than just the treated one. This diffuse pain pattern indicates that infection has spread into the surrounding tissues and bone structure.
Visible Changes and Swelling
When infection spreads to the jaw, visible external changes often occur. You might notice swelling that extends beyond the gum line to involve your cheek, jaw, or even down into your neck. The affected area may appear red or discolored, and the skin may feel tight and warm to the touch.
Lymph nodes in your neck may become swollen and tender as your immune system responds to the infection. These enlarged lymph nodes feel like tender lumps along the sides of your neck or under your jaw.
Systemic Symptoms
As jaw infections can become serious quickly, they often trigger whole-body symptoms including fever of 100.4°F (38°C) or higher, chills or night sweats, general feeling of being unwell or fatigued, and in severe cases, difficulty breathing or swallowing. These systemic symptoms indicate that the infection is affecting your entire body and requires urgent medical attention.
Understanding Root Canal Infection Development Timeline
The timing of symptom onset provides important clues about the nature and cause of the infection. Root canal infection can develop at different stages after treatment, each with distinct characteristics and implications.
Immediate Post-Procedure Period (Days 1-3)
During the first few days after treatment, some discomfort, sensitivity, and mild swelling are completely normal as your body heals from the procedure. This normal healing response includes mild to moderate pain that improves with over-the-counter pain medication, slight tenderness when biting on the treated tooth, and minor swelling that peaks around day two and then gradually decreases.
Symptoms during this period that suggest actual infection rather than normal healing include pain that intensifies rather than improves, severe swelling that develops quickly, presence of pus or foul taste, or fever and systemic symptoms. If you experience these concerning signs in the immediate aftermath of your procedure, contact your dentist promptly.
Short-Term Period (Days 4-14)
By the end of the first week, most normal post-treatment discomfort should be significantly improved or resolved. If symptoms persist or worsen during the second week, this strongly suggests infection or another complication. The temporary filling may have become compromised during this period, allowing bacterial contamination.
New symptoms developing during this timeframe especially after a period of feeling better—often indicate that bacteria have established an infection in the treated tooth or surrounding tissues.
Long-Term Period (Weeks to Months Later)
Sometimes infection doesn’t become apparent until weeks or even months after the root canal procedure. This delayed presentation often results from bacteria that were sealed inside the tooth due to complex canal anatomy, gradual breakdown of the seal allowing new bacterial entry, or development of a crack in the tooth that creates a pathway for bacteria.
Late-developing infections emphasize the importance of completing the final restoration (crown or filling) promptly after root canal therapy and maintaining regular dental checkups to monitor the treated tooth over time.
Diagnostic Methods for Detecting Root Canal Infections
When you visit your Dentist in Northampton, MA or any dental professional with concerns about post-treatment infection, they will use several diagnostic methods to assess your situation and determine if infection is present.
Clinical Examination
Your dentist will perform a thorough examination of the treated tooth and surrounding tissues. This includes visual inspection of the tooth and gums for signs of swelling, redness, or discharge, percussion testing (gently tapping the tooth) to assess sensitivity and pain response, palpation of the surrounding gums and tissues to check for tenderness or abnormalities, and assessment of the temporary or permanent restoration to ensure it’s intact and properly sealed.
The dentist will also review your symptoms in detail, asking about the onset, duration, character, and progression of any pain or other issues you’re experiencing.
Radiographic Evaluation
X-rays are essential for detecting infections that may not be visible during clinical examination. Periapical X-rays show the entire tooth including the root tips and surrounding bone, revealing signs of infection such as bone loss around the root tip (periapical radiolucency), inadequate canal filling that doesn’t extend to the root apex, or presence of cracks or perforations in the root.
Sometimes advanced imaging like cone beam CT scans may be necessary to fully evaluate complex situations, particularly if the infection has spread significantly or if unusual anatomy is suspected.
Additional Testing
In some cases, additional diagnostic procedures help confirm infection and guide treatment. These might include vitality testing on adjacent teeth to ensure they haven’t been affected, bacterial culture if antibiotic resistance is a concern, or referral to an endodontist (root canal specialist) for expert evaluation of complex cases.
Root Canal Infection Treatment Options
When infection is diagnosed, several root canal infection treatment approaches are available depending on the severity and cause of the infection. Your dentist will recommend the most appropriate option for your specific situation.
Antibiotic Therapy
Antibiotics play an important role in managing dental infections, particularly when there’s spreading infection, systemic symptoms like fever, or involvement of surrounding tissues. Common antibiotics prescribed for dental infections include amoxicillin, clindamycin (for patients allergic to penicillin), or metronidazole in combination with other antibiotics.
However, antibiotics alone cannot cure an infection inside the sealed root canal system because the medication cannot reach bacteria protected inside the tooth. Antibiotics serve to control spreading infection and reduce symptoms while definitive treatment is performed.
Root Canal Retreatment
When infection persists or recurs after initial treatment, retreatment (also called endodontic retreatment) is often the best option. This procedure involves removing the previous filling material from the canals, thoroughly cleaning and disinfecting the canal system again with enhanced techniques, addressing any previously missed canals or areas, and resealing the tooth with new filling material.
Retreatment has a good success rate, particularly when performed by an endodontist using advanced techniques like dental microscopes and ultrasonic instruments. The procedure is similar to the original root canal but focuses on correcting whatever factors led to the initial treatment failure.
Apicoectomy (Root-End Surgery)
When infection persists at the tip of the root despite retreatment, or when retreatment isn’t feasible due to posts or other factors, an apicoectomy may be recommended. This surgical procedure involves making a small incision in the gum tissue to access the infected area, removing the tip of the tooth root along with infected tissue, and sealing the end of the root with a biocompatible material.
Apicoectomy is typically performed by oral surgeons or endodontists and offers another opportunity to save the tooth when conventional retreatment cannot resolve the infection.
Tooth Extraction
In some cases, the infection cannot be resolved, or the tooth structure is too compromised to save. Extraction becomes necessary when there’s extensive root fracture that cannot be repaired, severe bone loss around the tooth that compromises stability, or persistent infection that doesn’t respond to multiple treatment attempts.
Following extraction, replacement options including dental implants, bridges, or partial dentures can restore both function and appearance. While losing the tooth is disappointing, extraction eliminates the source of infection and protects your overall health.
Preventing Infection After Root Canal Treatment
While not all post-treatment infections can be prevented, following proper care guidelines significantly reduces your risk and promotes successful healing.
Following Post-Treatment Instructions
Your dentist will provide specific care instructions after your root canal. Following these carefully is crucial for preventing complications. Key instructions typically include taking all prescribed medications exactly as directed, avoiding chewing on the treated tooth until the permanent restoration is placed, maintaining excellent oral hygiene while being gentle around the treated area, and attending all follow-up appointments as scheduled.
Don’t hesitate to contact your dentist if you have questions about any aspect of your post-treatment care or if symptoms concern you.
Completing the Final Restoration Promptly
One of the most important factors in preventing infection is placing the permanent crown or filling promptly after root canal therapy. The temporary filling used immediately after treatment is not designed for long-term protection and can break down or become loose if left in place too long.
Most dentists recommend completing the permanent restoration within a few weeks of the root canal procedure. This permanent seal prevents bacteria from re-entering the cleaned canal system and provides strength to protect the tooth from fracture.
Maintaining Good Oral Hygiene
Excellent oral hygiene helps prevent new infections and supports healing. Brush twice daily with fluoride toothpaste, floss daily (being gentle around the treated tooth initially), use an antimicrobial mouthwash if recommended by your dentist, and avoid tobacco products which impair healing.
Regular dental cleanings and checkups allow your dentist to monitor the treated tooth and address any early signs of problems before they become serious.
Protecting Your Treated Tooth
Root canal treated teeth are more brittle than healthy teeth because they no longer have a living pulp supplying moisture and nutrients. Protect your treated tooth by avoiding chewing extremely hard foods like ice, hard candies, or unpopped popcorn kernels, not using your teeth as tools to open packages or bottles, wearing a mouthguard if you grind your teeth at night, and having a crown placed on the tooth if recommended by your dentist.
When to Seek Immediate Dental Care
Certain symptoms indicate serious infection requiring urgent attention. Contact your dentist immediately or seek emergency care if you experience severe, uncontrolled pain that doesn’t respond to medication, significant facial swelling that’s rapidly worsening, fever above 101°F (38.3°C), difficulty breathing or swallowing, or swelling that extends to your eye, neck, or throat.
These symptoms can indicate a spreading infection that could become life-threatening if not treated promptly. Don’t wait for regular office hours if you experience severe symptoms—seek emergency dental care or go to a hospital emergency room.
The Importance of Regular Follow-Up Care
Even when you’re not experiencing symptoms, regular follow-up care is essential for monitoring the long-term success of your root canal treatment. Most dentists recommend X-rays of treated teeth at regular intervals to check for signs of infection or other complications that may develop without obvious symptoms.
These checkups allow early detection of problems when they’re easier to treat and before they cause pain or more serious complications. Never skip recommended follow-up appointments, even if you feel fine.
Conclusion
While root canal infection after treatment is relatively uncommon, being aware of the warning signs ensures you can recognize problems early and seek appropriate care. Understanding the difference between normal post-treatment discomfort and concerning symptoms of infection empowers you to take action when needed while avoiding unnecessary anxiety about the normal healing process.
Root canal treatment remains one of the most successful procedures in dentistry, saving countless teeth that would otherwise require extraction. When complications do occur, modern dentistry offers effective solutions ranging from antibiotics and retreatment to surgical approaches. The key is maintaining awareness, following care instructions carefully, and communicating promptly with your dental provider about any concerns.
Remember that your dentist is your partner in oral health and wants to ensure the success of your treatment. Don’t hesitate to reach out with questions or concerns early intervention for post-treatment complications almost always leads to better outcomes than waiting until problems become severe.
FAQs
How to treat tooth infection after root canal?
Treatment depends on the infection’s severity and cause. Your dentist will typically prescribe antibiotics to control spreading infection and reduce symptoms. Definitive treatment usually requires root canal retreatment to remove the previous filling, thoroughly re-clean the canals, and reseal the tooth. In some cases, an apicoectomy (surgical removal of the root tip) may be needed. Extraction is the last resort when the tooth cannot be saved. Complete the permanent crown or filling promptly if not already done, as this prevents reinfection.
Is it common to get an infection after a root canal?
No, infection after root canal is relatively uncommon. Root canal treatment has approximately a 95% success rate, meaning only about 5% of cases develop complications like infection. When infection does occur, it’s usually due to complex canal anatomy that prevented complete cleaning, compromised seals allowing bacterial reentry, or delayed placement of the permanent restoration. Following your dentist’s care instructions and completing the final crown or filling promptly significantly reduces infection risk.
How do I know if a root canal is infected?
Key signs include persistent or worsening pain beyond one week after treatment, swelling in the gums or face that develops or doesn’t improve, presence of pus or foul-tasting discharge from the gum, a pimple-like bump on the gum near the tooth, fever or feeling generally unwell, and sensitivity that intensifies rather than improves. If you experience any of these symptoms, contact your dentist promptly for evaluation. X-rays may reveal infection at the root tip not visible externally.
Do you need antibiotics after a root canal?
Antibiotics are not routinely prescribed after root canal treatment for all patients. Your dentist will prescribe antibiotics if you have significant infection or swelling before the procedure, symptoms of spreading infection, certain medical conditions that increase infection risk, or if infection develops after the procedure. Many successful root canals require no antibiotics because the procedure itself removes infected tissue and bacteria. Always take prescribed antibiotics exactly as directed, completing the full course even if symptoms improve.
What happens if a root canal becomes infected after the procedure?
If infection develops, the bacteria can spread to surrounding tissues and bone, potentially causing abscesses, bone loss, or systemic infection if untreated. Your dentist will evaluate the situation and typically recommend retreatment to re-clean the canals and eliminate infection. Antibiotics may be prescribed to control spreading infection. In cases where retreatment isn’t successful or feasible, apicoectomy (root-end surgery) or extraction may be necessary. Early detection and treatment prevent more serious complications and usually save the tooth.