Root canal treatment is one of the most common dental procedures performed to save a tooth that has become severely infected or damaged. While root canals have a high success rate typically around 85-97% complications can occasionally occur. Understanding the warning signs of infection after root canal treatment is crucial for protecting your oral health and ensuring the long-term success of your procedure.
Many patients wonder what’s normal during recovery and what signals a problem. While some discomfort is expected in the first few days following treatment, certain symptoms should never be ignored. This comprehensive guide will help you identify the six most important warning signs that may indicate an infection has developed after your root canal procedure, along with actionable steps you can take to address these concerns.
Understanding Root Canal Infections
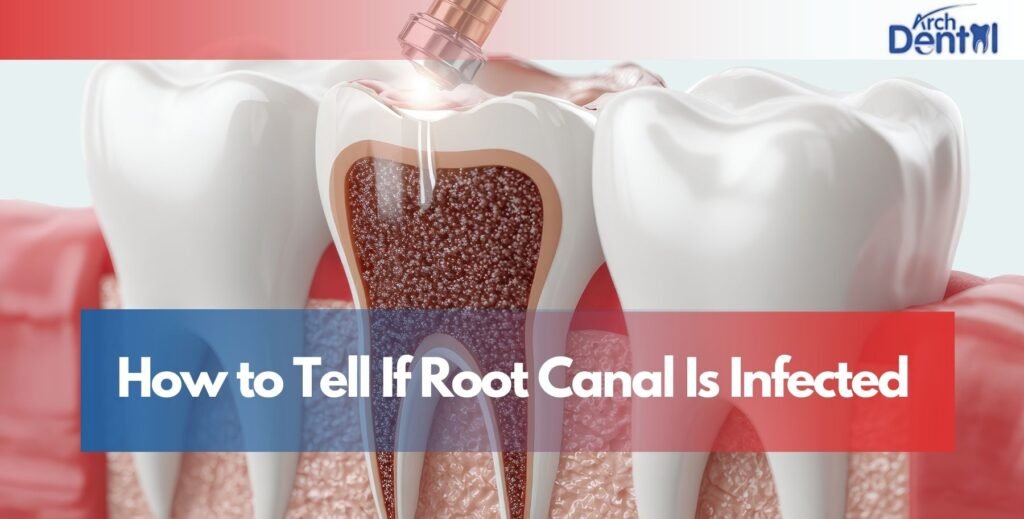
Before diving into the specific warning signs, it’s helpful to understand why infections can occur even after a root canal. During the procedure, your dentist removes infected pulp tissue from inside the tooth, cleans and disinfects the canals, and seals them to prevent future bacterial invasion. However, infections can still develop for several reasons: incomplete removal of bacteria, new bacterial entry through a compromised seal, cracks in the tooth structure, or delayed placement of a permanent crown.
The body’s immune response to lingering bacteria can cause inflammation and discomfort that extends beyond normal post-treatment healing. Recognizing these signs early allows for prompt intervention, which significantly improves treatment outcomes and prevents complications from spreading to surrounding tissues or your bloodstream.
Sign 1: Unusual Taste Sensations
One of the earliest indicators that something isn’t right after your root canal is experiencing strange taste sensations in your mouth. A metallic taste in the mouth after root canal can occur for various reasons, some benign and others concerning. Immediately following treatment, a slight metallic or medicinal taste from dental materials or medications used during the procedure is relatively normal and should fade within 24-48 hours.
However, if you notice a bad taste in the mouth after root canal temporary filling that persists or worsens after the first few days, this warrants attention. This unpleasant taste often results from bacteria accumulating around the temporary filling or seeping from beneath it if the seal has become compromised. A funny taste in the mouth after root canal combined with other symptoms like swelling or pain suggests active bacterial growth that requires professional evaluation.
When Taste Changes Signal Trouble
Pay particular attention if the bad taste in the mouth after root canal is accompanied by drainage, pus, or a foul odor. These are clear indicators of infection. Similarly, a metallic taste after root canal that develops suddenly after several days or weeks of normal healing should prompt an immediate call to your dentist. A weird taste in the mouth after root canal that’s described as bitter, sour, or simply “off” often indicates bacterial byproducts and should not be dismissed as insignificant.
The presence of a metallic taste in the mouth root canal specifically may relate to the materials used in your treatment or could signal tissue inflammation. When this persists beyond the initial recovery period, it’s essential to have your dentist examine the treated tooth to ensure the restoration remains intact and no infection is developing.
Sign 2: Persistent or Worsening Pain
While moderate discomfort is expected for 3-5 days after a root canal, pain should gradually decrease each day. If you experience sharp, throbbing, or intensifying pain beyond this initial period, it may indicate infection. Symptoms of jaw infection after root canal can include pain that radiates to your jaw, ear, or neck, making it difficult to chew or fully open your mouth.
Pain that disrupts sleep, requires increasing doses of pain medication, or feels disproportionate to what you’d expect from healing tissues deserves immediate professional attention. Some patients describe the sensation as pressure building inside the tooth or surrounding bone, which can signal abscess formation. Trust your instincts if the pain feels wrong or different from what your dentist described as normal, don’t hesitate to call for guidance.
Distinguishing Normal Discomfort from Infection Pain
Normal post-root canal discomfort typically presents as tenderness when biting or mild sensitivity that responds well to over-the-counter pain relievers. Infection pain, by contrast, often feels more intense, constant, and throbbing in nature. It may wake you at night and doesn’t significantly improve with standard pain management techniques. This type of pain frequently accompanies other infection signs like swelling or fever.
Sign 3: Swelling and Visible Gum Changes
Swelling is one of the most visible signs of infection and should never be ignored. Minor gum tenderness immediately around the treated tooth is normal for the first few days, but pronounced swelling that extends to your face, jaw, or neck indicates a serious problem. A bump on gum months after root canal is particularly concerning, as this often represents an abscess, a pocket of infection that has formed near the tooth root.
Gum infection after root canal treatment may present as red, inflamed tissue that appears shiny or stretched. The gums might feel hot to the touch and could bleed easily when you brush. Some patients notice a pimple-like bump on their gum tissue that may intermittently drain a foul-tasting fluid, temporarily relieving pressure before refilling. This drainage bump, called a fistula, is a definitive sign of ongoing infection that requires treatment.
When to Seek Emergency Care for Swelling
If swelling progresses rapidly, extends to your eye or neck, or makes breathing or swallowing difficult, seek emergency dental care immediately. These symptoms can indicate a spreading infection that could become life-threatening. Even moderate swelling that persists beyond five days post-treatment should be evaluated, as it suggests the body cannot overcome the infection without intervention.
Sign 4: Fever and Systemic Symptoms
A low-grade fever (under 100°F) for 24-48 hours after your root canal can be normal as your body responds to the procedure. However, a fever that persists beyond this timeframe, reaches 101°F or higher, or develops days or weeks after treatment signals systemic infection. Your body is fighting bacteria that may be spreading beyond the localized treatment area.
Other systemic symptoms to watch for include general malaise, unusual fatigue, chills, or feeling “flu-like” without actually having the flu. These signs indicate your immune system is working overtime to combat infection. Some patients also experience swollen lymph nodes in their neck or under their jaw, which becomes tender to touch. These nodes enlarge as they filter bacteria and produce immune cells to fight infection.
Sign 5: Drainage and Pus Formation
The presence of pus is an unmistakable sign of infection. You might notice yellow, white, or greenish discharge around the treated tooth, which often has an unpleasant odor and taste. This drainage can be constant or intermittent, and you may notice it particularly when pressing on the surrounding gum tissue.
Some patients first become aware of drainage when they wake up with a bad taste in their mouth or notice staining on their pillow. The pus represents dead white blood cells, bacteria, and tissue debris from your body’s battlefield waste from fighting infection. Any visible drainage requires prompt dental evaluation, as it indicates active infection that won’t resolve without professional treatment.
Understanding Abscess Formation
An abscess develops when infection becomes walled off by your body’s immune response, creating a pocket filled with pus. This can occur at the tooth’s root tip (periapical abscess) or in the surrounding gum tissue (periodontal abscess). Abscesses can be extremely painful and may cause visible facial swelling. They require drainage and antimicrobial treatment to resolve completely.
Sign 6: Tooth Discoloration or Increased Mobility
A tooth that darkens significantly after a root canal may indicate blood vessel damage or tissue necrosis inside the tooth structure. While some minimal darkening can occur naturally, dramatic color changes particularly when accompanied by other symptoms may signal ongoing infection or treatment failure. The tooth might appear grayish, brownish, or have a notably different shade compared to adjacent teeth.
Increased tooth mobility is another serious warning sign. Your treated tooth should feel stable and secure in its socket. If you notice it feels loose, shifts when you touch it with your tongue, or moves when you bite down, this suggests bone loss around the root from infection. The surrounding periodontal ligament and bone structure may be deteriorating due to persistent bacterial activity.
What to Do If You Suspect Infection
If you recognize any of these warning signs, contact your dentist immediately. Don’t wait for symptoms to worsen or hope they’ll resolve on their own. Your dentist will likely want to see you for an examination, which may include X-rays to assess the bone around your tooth root and evaluate the quality of the root canal filling. Treatment options depend on the infection’s severity and may range from antibiotics and improved oral hygiene to retreatment of the root canal or, in severe cases, extraction.
Time is critical when dealing with dental infections. What begins as a localized problem can spread to surrounding tissues, your jawbone, or even your bloodstream if left untreated. Early intervention not only saves your tooth but prevents potentially serious health complications.
Conclusion
Recognizing the signs of infection after root canal treatment empowers you to take swift action when problems arise. While most root canals heal without complications, staying vigilant for unusual taste sensations, persistent pain, swelling, fever, drainage, or changes in your tooth’s appearance ensures any developing infection receives prompt attention. Your oral health directly impacts your overall wellbeing, making it essential to address concerning symptoms rather than dismissing them as normal healing.
If you’re experiencing any of these warning signs or have concerns about your root canal recovery, the experienced team at your trusted Dentist in Northampton, MA is here to help. Professional evaluation and timely treatment can make the difference between saving your tooth and facing more extensive dental work. Never hesitate to reach out when something doesn’t feel right—your dental professionals would much rather examine you and find nothing wrong than have you wait until a minor problem becomes a major complication.
Frequently Asked Questions
Can a root canal cause nausea?
Yes, nausea can occasionally occur after a root canal, typically due to swallowing blood during the procedure, anxiety, pain medication side effects, or in rare cases, infection spreading and triggering a systemic response. If nausea persists beyond 24 hours or is accompanied by fever, contact your dentist.
How to relieve root canal pain while pregnant?
Pregnant patients should use acetaminophen (Tylenol) as directed by their dentist or obstetrician, as it’s generally considered safe during pregnancy. Apply cold compresses to the outside of your cheek, keep your head elevated, and avoid lying flat. Contact your dentist for severe pain, as some prescription options may be appropriate during pregnancy.
Can a root canal cause ear pain?
Yes, ear pain after a root canal is relatively common due to shared nerve pathways between your teeth and ears. The trigeminal nerve serves both areas, so inflammation from dental treatment can create referred pain in your ear. This should resolve within a few days; persistent ear pain may indicate infection.
Can a tooth infection cause diarrhea?
While uncommon, a severe tooth infection that spreads systemically can cause gastrointestinal symptoms including diarrhea as your body fights the bacterial invasion. More commonly, antibiotics prescribed to treat the infection cause diarrhea as a side effect by disrupting normal intestinal bacteria.
How do you know if a tooth infection has spread to your body?
Warning signs include high fever (over 101°F), rapid swelling extending to your neck or face, difficulty breathing or swallowing, severe fatigue, confusion, rapid heart rate, or feeling seriously ill. These symptoms indicate a potentially life-threatening condition requiring immediate emergency medical attention.