Receiving a diagnosis of periodontal disease can feel devastating, leaving many patients wondering if they’re destined to lose their teeth or if maintaining an attractive smile is still possible. The good news is that with proper treatment and diligent care, you absolutely can preserve beautiful, functional teeth even after developing gum disease. While periodontitis is a serious condition that damages the gums and bone supporting your teeth, modern dental treatments combined with committed home care can halt disease progression and restore oral health. Understanding how to manage this condition effectively empowers you to keep your natural teeth looking great for years to come. This comprehensive guide explores how periodontal disease affects your smile, what treatments can restore gum health, and the steps you can take to maintain attractive teeth despite this common dental condition.
Understanding Periodontal Disease and Its Effects
Periodontal disease progresses through distinct stages, each affecting your teeth and gums differently, making early detection and treatment critical for preserving your smile’s appearance and function.
What Happens During Gum Disease
Gum disease begins when bacteria accumulate along the gum line, forming sticky plaque that hardens into tartar if not removed through brushing and flossing. This bacterial buildup triggers inflammation as your immune system responds to the infection, causing gums to become red, swollen, and prone to bleeding. As inflammation persists, the gums pull away from teeth, creating periodontal pockets where more bacteria accumulate in spaces your toothbrush cannot reach. The infection progressively destroys the connective tissue and bone that anchor your teeth in place. Without intervention, this destruction continues silently often without pain until teeth become loose or fall out. The visible effects include receding gums that make teeth appear longer, spaces developing between teeth, and changes in bite alignment.
Early Stage Gingivitis Versus Advanced Periodontitis
Gingivitis represents the earliest and most reversible stage of gum disease, characterized by inflammation confined to the gum tissue without bone loss. Your gums may bleed when brushing or flossing, appear puffy or red, and feel tender, but no permanent damage has occurred yet. Professional cleaning combined with improved home care can completely reverse gingivitis, restoring healthy gums. In contrast, advanced periodontitis involves significant bone destruction, deep periodontal pockets (6mm or deeper), loose teeth, and sometimes pus discharge. The damage from periodontitis is permanent lost bone that doesn’t regenerate naturally though treatment can stabilize the condition and prevent further deterioration. Understanding this distinction highlights why catching gum disease early dramatically improves your chances of keeping attractive, healthy teeth.
How Periodontal Disease Affects Tooth Appearance
Beyond health concerns, periodontal disease creates aesthetic problems that affect your smile’s appearance. Gum recession exposes tooth roots, making teeth look unnaturally long and creating a “toothy” appearance. Exposed roots often appear yellower than the white enamel covering tooth crowns, creating an uneven color. Spaces develop between teeth as bone loss allows them to shift positions. Swollen, inflamed gums appear bright red instead of healthy pink, drawing unwanted attention. Severe cases involve visible gum pockets filled with debris, and teeth may appear to tilt or lean as bone support diminishes. Chronic inflammation can cause gum tissue to thicken and become irregular in texture. These cosmetic concerns often motivate patients to seek treatment even before functional problems develop.
The Connection Between Gum Health and Overall Appearance
Your gum health significantly impacts not just individual teeth but your entire facial appearance and smile aesthetics. Healthy gums frame your teeth like a picture frame, with symmetrical contours and consistent pink color enhancing the whiteness of teeth. Periodontal disease disrupts this harmony, creating an aged appearance as receding gums mimic the natural gum loss that occurs with aging. Severe bone loss can change facial structure over time, causing the lower face to appear shortened and the lips to lose support. The inflammation and infection also contribute to bad breath that affects social interactions. Fresh breath and healthy pink gums convey youth, vitality, and good hygiene. Restoring gum health through periodontal treatment reverses many of these aesthetic concerns, helping you look and feel your best.
Why Early Intervention Makes a Huge Difference
Addressing gum disease in its earliest stages prevents the permanent damage that compromises both function and appearance of your teeth. Early-stage periodontal disease responds dramatically to professional cleaning and improved oral hygiene, often resolving completely within weeks. Catching the condition before significant bone loss occurs means your teeth retain full support and stability, with gums that can return to normal contours. Delayed treatment allows progressive bone destruction that cannot be fully reversed, even with the best interventions. Patients who address gum disease early maintain natural tooth positioning, avoid surgical interventions, and preserve their attractive smile with minimal intervention. Regular dental checkups detect gum disease in its earliest, most treatable stages, making preventive care your best strategy for keeping nice teeth throughout life.
Professional Treatments That Restore Gum Health
Modern periodontal treatments offer effective solutions for managing gum disease at every stage, from non-surgical approaches for early disease to advanced procedures for severe cases.
Deep Cleaning (Scaling and Root Planing)
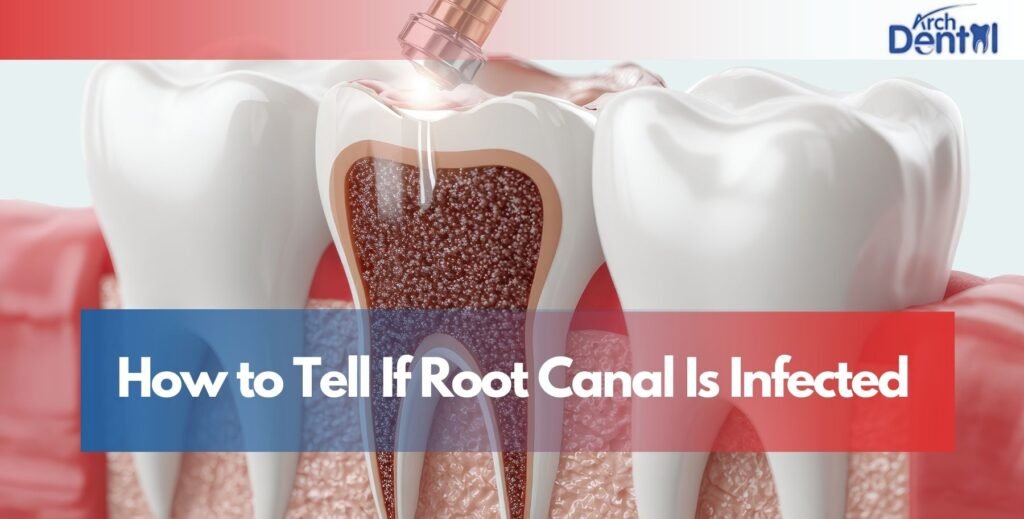
Scaling and root planing represents the gold standard first-line treatment for periodontal disease, thoroughly cleaning below the gum line where your toothbrush cannot reach. During scaling, your dental hygienist or periodontist uses specialized instruments to remove plaque and tartar deposits from tooth surfaces and beneath the gums, clearing away the bacterial colonies causing infection. Root planing smooths the tooth root surfaces, eliminating rough areas where bacteria cling and encouraging gums to reattach to clean tooth surfaces. The procedure is typically performed under local anesthesia over 2-4 appointments, treating one section of your mouth at a time for comfort. Deep cleaning reduces pocket depths, eliminates bleeding and inflammation, and halts bone loss progression. Many patients notice dramatic improvements in gum appearance and health within weeks, with pink, firm gums replacing inflamed, bleeding tissue.
Antibiotic Therapy for Infection Control
Antibiotic treatment complements deep cleaning by targeting the specific bacteria responsible for periodontal infection, enhancing treatment success rates. Your dentist may place antibiotic chips, gels, or microspheres directly into periodontal pockets, delivering concentrated medication exactly where infection exists. These local antibiotics release slowly over days or weeks, maintaining therapeutic levels that kill bacteria. Oral antibiotics taken as pills provide systemic treatment for widespread or aggressive periodontal disease, though they’re typically reserved for severe cases or patients with compromised immune systems. The combination of mechanical cleaning plus antibiotics produces better results than either approach alone. Your gum tissue responds by becoming firmer, pinker, and less prone to bleeding as the infection resolves, improving both health and appearance of your smile.
Laser Gum Treatment
Laser periodontal therapy offers a minimally invasive alternative to traditional gum surgery, using focused light energy to remove diseased gum tissue and kill bacteria. The laser targets only infected tissue, preserving healthy gums and promoting faster healing with less discomfort than conventional surgery. Laser treatment stimulates tissue regeneration and blood clot formation that encourages gum reattachment to teeth. Patients experience minimal bleeding, reduced swelling, and quicker recovery compared to traditional surgical approaches. The precision of laser technology allows treatment of specific problem areas without affecting adjacent healthy tissues. Many patients prefer laser therapy because it typically doesn’t require cutting or sutures, and discomfort during and after treatment is minimal. The aesthetic results are often excellent, with gums that heal into natural contours and healthy pink color.
Gum Grafting for Recession
Gum recession exposes tooth roots, creating both aesthetic concerns and sensitivity problems that gum grafting surgery can address effectively. During gum graft procedures, tissue is taken from the roof of your mouth or obtained from a tissue bank and attached to areas with insufficient gum coverage. The grafted tissue covers exposed roots, eliminates sensitivity, and restores a more natural gum line that enhances your smile’s appearance. The procedure protects tooth roots from decay and further recession while improving the symmetry and balance of your gum tissue. Healing takes several weeks, after which the grafted tissue becomes indistinguishable from your natural gums. Multiple teeth can be treated in one surgical session. Gum grafting transforms smiles affected by recession, restoring youthful proportions and reducing the “long tooth” appearance that bothers many periodontal disease patients.
Bone Regeneration Procedures
Advanced periodontal disease destroys the bone supporting your teeth, but bone grafting and regeneration procedures can rebuild some of this lost structure. During surgery, your periodontist cleans infected areas, then places bone graft material—either your own bone, processed donor bone, or synthetic materials—into defects where bone has been lost. Growth factors and specialized membranes that encourage bone formation may be added to enhance results. Over several months, your body gradually replaces the graft material with new natural bone, restoring support for teeth. This regenerative treatment can reduce pocket depths, stabilize loose teeth, and improve the foundation supporting your smile. While not all lost bone can be regenerated, these procedures often restore significant structure, preventing tooth loss and creating conditions where gum tissue can return to health. The improved bone support helps maintain natural tooth positioning and bite alignment.
Daily Care Strategies for Managing Periodontal Disease
Controlling gum disease at home requires specific techniques and commitment beyond basic brushing, making your daily oral hygiene routine the foundation of successful periodontal management.
Proper Brushing Techniques for Diseased Gums
Brushing with periodontal disease requires extra attention to the gum line where bacteria accumulate, using gentle technique that cleans effectively without causing trauma. Use a soft-bristled toothbrush or electric toothbrush with a pressure sensor to avoid damaging already compromised gum tissue. Angle the bristles at 45 degrees toward the gum line, allowing bristles to reach slightly under the gums where plaque hides. Use small circular or vibratory motions rather than aggressive back-and-forth scrubbing that can worsen recession. Spend at least 30 seconds on each section of your mouth, ensuring thorough cleaning of all tooth surfaces. Replace your toothbrush every 6-8 weeks or sooner if bristles become frayed. Electric toothbrushes often prove more effective for periodontal patients, removing more plaque with less effort and trauma to tissues.
Advanced Flossing and Interdental Cleaning
Flossing becomes absolutely critical when you have periodontal disease, as bacteria between teeth and below the gum line fuel disease progression. Use proper flossing technique by curving the floss around each tooth in a “C” shape and sliding it gently beneath the gum line, cleaning both sides of every tooth. Interdental brushes in various sizes clean effectively between teeth and are often easier to use than traditional floss for patients with large spaces or manual dexterity challenges. Water flossers (oral irrigators) provide excellent cleaning for periodontal pockets, flushing bacteria and debris from areas difficult to reach with floss. Some water flossers have special tips designed specifically for periodontal disease treatment. Clean between all teeth at least once daily preferably before bed—to remove the day’s accumulation of food particles and bacteria. Your dental hygienist can demonstrate the most effective techniques for your specific situation.
Antimicrobial Rinses and Special Products
Prescription mouthwashes containing chlorhexidine or other antimicrobial agents significantly reduce bacteria levels in your mouth, supporting gum disease treatment. Your dentist may prescribe these rinses for daily use over weeks or months, particularly following deep cleaning or surgery. Over-the-counter rinses with essential oils or cetylpyridinium chloride also help control bacteria, though they’re less potent than prescription options. Avoid alcohol-based rinses that can dry and irritate already inflamed gum tissue. Some patients benefit from specialized periodontal gels applied directly to diseased areas, delivering concentrated medication to stubborn pockets. Fluoride rinses or gels strengthen tooth surfaces exposed by gum recession, preventing root cavities. Your dental team recommends specific products based on your disease severity and individual needs, creating a customized home care regimen that maximizes treatment success.
Dietary Choices That Support Gum Health
Your diet impacts periodontal disease progression, with certain foods supporting healing while others worsen inflammation and bacterial growth. Reduce consumption of sugary and starchy foods that feed harmful bacteria, choosing instead fresh vegetables, lean proteins, and dairy products that support oral health. Foods rich in vitamin C citrus fruits, berries, bell peppers promote gum tissue healing and collagen formation. Omega-3 fatty acids from fish, walnuts, and flaxseed reduce inflammation throughout your body, including your gums. Crunchy vegetables like carrots and celery provide natural teeth cleaning action. Stay well-hydrated, as adequate saliva flow helps wash away bacteria and neutralize acids. Limit acidic foods and beverages that can irritate inflamed gum tissue. A nutrient-rich diet supports your immune system’s ability to fight infection and heal damaged tissues, complementing your oral hygiene efforts.
Avoiding Habits That Worsen Periodontal Disease
Certain lifestyle habits dramatically undermine periodontal treatment success, making their elimination essential for preserving your teeth. Smoking is the single most destructive habit for gum health, reducing blood flow to gums, impairing healing, and increasing infection risk. Smokers respond poorly to periodontal treatment and experience much higher rates of tooth loss. Quitting smoking provides immediate benefits for gum health and treatment outcomes. Stress contributes to periodontal disease by suppressing immune function and often leading to poor oral hygiene practices and teeth grinding. Managing stress through exercise, meditation, or counseling supports your oral health. Teeth grinding (bruxism) places excessive force on already compromised teeth; wearing a nightguard protects them from this damage. Avoiding these harmful habits gives your periodontal treatment the best chance of success, helping you maintain attractive, healthy teeth.
Cosmetic Solutions for Teeth Affected by Gum Disease
Even after successfully treating periodontal disease, aesthetic concerns may remain that cosmetic dentistry can address, restoring your confidence in your smile’s appearance.
Addressing Gum Recession and Uneven Gum Lines
Cosmetic gum surgery (gingivoplasty or crown lengthening) reshapes gum tissue to create symmetrical, aesthetically pleasing contours that enhance your smile. For patients with uneven gum lines resulting from periodontal disease, this procedure removes excess tissue or sculpts gums to achieve balance. Gum contouring can eliminate the “gummy smile” appearance or correct irregularities caused by disease. The procedure is typically performed with lasers or electrosurgery that sculpt tissue precisely while minimizing bleeding and discomfort. Healing takes 1-2 weeks, after which your gums display natural, symmetrical contours that showcase your teeth attractively. Combined with gum grafting where recession has occurred, cosmetic gum surgery transforms smiles compromised by periodontal disease. The results look completely natural, with no one suspecting you’ve had gum problems in the past.
Tooth-Colored Restorations for Exposed Roots
Exposed tooth roots from gum recession often appear yellow or discolored compared to the white enamel on tooth crowns, creating an uneven appearance. Composite bonding allows your dentist to cover exposed root surfaces with tooth-colored resin that matches your natural teeth perfectly. The material is sculpted directly onto the tooth, concealing discoloration and creating uniform color from gum line to biting edge. Bonding also eliminates the sensitivity that often accompanies root exposure. The procedure is quick, comfortable, and doesn’t require removing tooth structure or anesthesia in most cases. Results last several years with proper care. For more extensive damage or multiple affected teeth, porcelain veneers provide durable, stain-resistant coverage that completely transforms your smile. These thin shells cover the front surface of teeth, masking discoloration, chips, or irregular shapes resulting from periodontal disease.
Orthodontics to Correct Shifting Teeth
Periodontal disease often causes teeth to shift positions as bone support diminishes, creating gaps, crowding, or tilting that affects both function and appearance. Once gum disease is controlled and bone loss stabilized, orthodontic treatment can reposition teeth to their proper locations. Modern options include traditional braces, clear aligners, or accelerated orthodontics that achieve results in months rather than years. Straightening teeth doesn’t just improve aesthetics, it also makes them easier to clean effectively, reducing your risk of disease recurrence. Your orthodontist works closely with your periodontist to ensure tooth movement occurs safely without compromising periodontal health. The combination of successful periodontal therapy followed by orthodontics produces dramatic smile transformations, eliminating the telltale signs that gum disease ever affected your teeth.
Teeth Whitening After Periodontal Treatment
Professional teeth whitening brightens teeth discolored by years of staining or the natural yellowing that occurs with age, creating a vibrant smile following periodontal treatment. However, whitening must be carefully timed; gums need to be completely healthy before undergoing the procedure to avoid sensitivity and irritation. Your dentist may recommend waiting several months after completing periodontal therapy before whitening. Professional whitening performed in the dental office or with custom take-home trays provides dramatic results safely and predictably. Teeth bleaching works on natural tooth enamel but won’t change the color of exposed root surfaces, which may require bonding for uniform appearance. The psychological boost from a brighter smile often motivates patients to maintain excellent oral hygiene, protecting their investment in periodontal treatment.
Full Smile Makeovers for Comprehensive Transformation
For patients with extensive damage from advanced periodontal disease, a complete smile makeover addresses all aesthetic and functional concerns comprehensively. This approach combines multiple treatments, periodontal therapy, gum grafting, orthodontics, crowns, veneers, and whitening into a coordinated plan that transforms your smile completely. Your dental team uses digital smile design technology to show you potential results before treatment begins, allowing refinement of the plan to match your goals. Treatment is phased over months, addressing periodontal health first, then reconstructive work, and finally cosmetic enhancements. The investment is substantial, but the results are life-changing, providing a beautiful, healthy smile you’re proud to show. Many patients report that comprehensive smile restoration improves not just their oral health but their confidence, career success, and quality of life dramatically.
Maintaining Long-Term Success After Treatment
Successfully managing periodontal disease requires lifelong commitment to maintenance care that prevents recurrence and protects your investment in treatment.
Regular Periodontal Maintenance Visits
After completing active periodontal treatment, you’ll transition to periodontal maintenance cleanings scheduled every 3-4 months instead of the typical six-month interval. These specialized appointments involve thorough cleaning below the gum line, measurement of pocket depths to monitor disease status, and evaluation of your home care effectiveness. The more frequent schedule prevents bacterial recolonization of treated areas, catching any disease recurrence at the earliest possible stage. During these visits, your hygienist reinforces proper cleaning techniques and addresses any problem areas requiring extra attention. Periodontal maintenance is not optional, it’s essential for keeping your disease under control and preserving your teeth. Patients who maintain their recommended cleaning schedule retain their teeth at much higher rates than those who revert to less frequent visits.
Monitoring for Disease Recurrence
Periodontal disease is a chronic condition that can return if bacterial levels increase or your immune response changes, making vigilant monitoring essential. Your dental team tracks pocket depths, bleeding scores, and bone levels over time, comparing current measurements to previous visits. Any increases in pocket depths or return of bleeding indicates disease reactivation requiring intervention. You should also self-monitor, watching for warning signs like bleeding when brushing, gum swelling, bad breath, or teeth feeling loose. Report these symptoms immediately rather than waiting for your next scheduled appointment. Early detection of recurrence allows simple treatment adjustments before significant damage occurs. Some patients require additional deep cleaning or antibiotic therapy periodically to control stubborn areas. The good news is that with proper maintenance, most patients successfully control their disease indefinitely.
Adjusting Your Home Care as Needed
Your oral hygiene routine may need modification over time as your periodontal condition changes or as you age and face new challenges. Arthritis or other conditions affecting manual dexterity might require switching to electric toothbrushes or modified flossing tools. New periodontal pockets developing in specific areas need targeted cleaning with specialized brushes or floss threaders. Your dental hygienist provides updated instructions tailored to your current needs, demonstrating new techniques or products that improve your effectiveness. Some patients benefit from prescription toothpastes for sensitivity or special rinses for stubborn bacteria. Stay open to adjusting your routine based on professional recommendations and your own observations about what works best. The goal is maintaining optimal cleanliness in all areas of your mouth, particularly those vulnerable to disease recurrence.
Managing Medical Conditions Affecting Periodontal Health
Systemic health conditions like diabetes, heart disease, or autoimmune disorders significantly impact periodontal disease progression and treatment success. Managing these conditions optimally controlling blood sugar, taking prescribed medications, and maintaining healthy weight directly benefits your gum health. Inform both your dentist and physician about all health conditions and medications, as many drugs cause dry mouth or other side effects affecting oral health. Diabetes and periodontal disease have a bidirectional relationship each condition worsens the other making control of both critical. Some medications like bisphosphonates for osteoporosis complicate certain dental procedures, requiring special precautions. Regular communication between your dental and medical providers ensures coordinated care that addresses your overall health comprehensively. Taking control of systemic health conditions provides your periodontal treatment the best chance for long-term success.
The Psychological Benefits of Maintaining Your Smile
Successfully managing periodontal disease and keeping your natural teeth provides profound psychological and social benefits beyond physical health. Your smile affects how others perceive you and how you feel about yourself, influencing confidence in social and professional situations. The knowledge that you’ve overcome a serious health challenge and preserved your teeth creates a sense of accomplishment and empowerment. You’re more likely to smile freely without self-consciousness about gum appearance or bad breath. Eating comfortably without pain or embarrassment about loose teeth improves your enjoyment of meals and social dining. The investment in maintaining your periodontal health pays dividends in quality of life, self-esteem, and overall wellbeing that extend far beyond dental considerations.
Conclusion
The answer to whether you can have nice teeth with periodontal disease is a resounding yes with proper treatment and committed maintenance care. While gum disease is serious and causes permanent changes to the structures supporting your teeth, modern periodontal treatments can halt progression, restore health, and address aesthetic concerns effectively. The key factors determining success are early intervention, following your dental team’s treatment recommendations, maintaining excellent home care, and committing to lifelong maintenance visits. Thousands of patients with periodontal disease keep their natural teeth looking beautiful for decades by taking these steps. Rather than viewing your diagnosis as a death sentence for your smile, consider it a wake-up call prompting the changes needed to preserve your teeth for life.
If you’re concerned about gum disease or want to preserve your smile despite periodontal challenges, consulting with an experienced dentist in Northampton, MA provides the professional evaluation and treatment planning you need. Local dental professionals offer comprehensive periodontal care and cosmetic solutions to help you maintain attractive, healthy teeth throughout your life.
Frequently Asked Questions
Can you have healthy teeth with periodontal disease?
Yes, you can have healthy teeth with periodontal disease through proper treatment and maintenance. While the disease damages gum and bone support, professional therapy halts progression, and excellent oral hygiene keeps teeth functional and attractive. Regular periodontal maintenance visits are essential for long-term success.
Can you still have nice teeth with gum disease?
Absolutely. Modern periodontal treatments restore gum health, while cosmetic procedures address aesthetic concerns like recession or discoloration. With commitment to professional care and daily oral hygiene, your teeth can look great despite having had gum disease. Many patients maintain beautiful smiles for decades after treatment.
Can I keep my teeth with advanced periodontal disease?
Yes, even advanced periodontal disease doesn’t automatically mean tooth loss. Aggressive treatment including deep cleaning, surgery, or bone grafting can stabilize the condition and save teeth. Success requires dedicated home care and regular professional maintenance. Many teeth with significant bone loss remain functional for years with proper management.
Do people with periodontal disease always lose their teeth?
No, tooth loss from periodontal disease is preventable with appropriate treatment and maintenance. Many patients successfully control their disease and keep their natural teeth throughout life. Untreated periodontal disease leads to tooth loss, but professional care and good oral hygiene stop progression in most cases.
Will removing teeth stop periodontal disease?
Removing teeth eliminates disease in those specific locations but doesn’t cure periodontal disease affecting remaining teeth. The bacteria causing periodontal disease remain in your mouth and can continue damaging other teeth. Extracting all teeth stops periodontal disease completely but leaves you requiring dentures or implants for replacement.
Is my life over if I have periodontitis?
Absolutely not. Periodontitis is a manageable chronic condition, not a life-ending diagnosis. Modern treatments are highly effective, and most patients successfully control their disease and keep their teeth. The key is taking action getting treatment, improving oral hygiene, and maintaining regular dental care. Many people live full, healthy lives while managing periodontitis.