Tooth pain can be one of the most distressing experiences, often leaving people wondering how long they’ll have to endure the discomfort. When a tooth’s nerve becomes damaged or infected, the pain can range from mild sensitivity to excruciating throbbing that disrupts daily life. Understanding the timeline of nerve damage and the eventual death of a tooth’s pulp is crucial for knowing when to seek dental treatment.
The duration of tooth pain before a nerve dies varies significantly from person to person, typically lasting anywhere from a few days to several months. However, the death of a tooth’s nerve doesn’t always mean the end of pain, and allowing a nerve to die without professional intervention can lead to serious complications.
Understanding Tooth Nerve Anatomy
The dental pulp, commonly referred to as the tooth’s nerve, sits at the center of each tooth and contains blood vessels, connective tissue, and nerve fibers. This soft tissue extends from the crown of the tooth down through the root canals. The pulp plays a vital role in tooth development and provides sensory function, alerting you to temperature changes, pressure, and damage.
When bacteria penetrate through tooth decay, cracks, or trauma, the pulp becomes inflamed in a condition called pulpitis. This inflammation triggers the immune response, causing swelling within the confined space of the tooth, which puts pressure on the nerve endings and creates intense pain.
Timeline of Tooth Pain and Nerve Death
Understanding the progression of dental nerve damage helps you recognize when to seek treatment and what symptoms to expect during each stage.
Early Stage: Reversible Pulpitis
In the initial stages of nerve damage, you may experience sharp, temporary pain when consuming hot, cold, or sweet foods and beverages. This stage, known as reversible pulpitis, can last for several days to weeks. At this point, the nerve is inflamed but still alive and potentially savable with appropriate dental treatment such as removing decay and placing a filling.
If treated promptly during this phase, the tooth’s nerve can heal and return to normal function. However, many people ignore these early warning signs, allowing the condition to progress.
Progressive Stage: Irreversible Pulpitis
When inflammation becomes severe, the condition advances to irreversible pulpitis. During this stage, pain becomes more intense, persistent, and spontaneous, often waking you from sleep. The discomfort may linger for minutes to hours after the stimulus is removed, and over-the-counter pain medications provide only temporary relief.
This phase typically lasts from several days to a few weeks, though some cases may extend to months. The pain pattern often intensifies before the nerve finally dies, with throbbing sensations that radiate to the jaw, ear, or surrounding teeth.
Final Stage: Nerve Necrosis
Eventually, the inflamed pulp tissue begins to die, a process called necrosis. As the nerve dies, many patients experience a temporary reduction or complete cessation of pain, leading them to mistakenly believe the problem has resolved itself. This pain-free period can last days or even weeks, creating a false sense of security.
However, the death of the tooth’s nerve is not the end of the problem. Dead tissue inside the tooth becomes a breeding ground for bacteria, leading to infection that can spread beyond the tooth root into the surrounding bone and tissues.
What Happens After the Nerve Dies
Many people mistakenly believe their dental problems are over when pain subsides, but nerve death often marks the beginning of more serious complications.
Dental Abscess Formation
After nerve death, bacterial infection often develops at the tooth’s root tip, forming a periapical abscess. This condition brings a new wave of pain, often more severe than the original toothache. Symptoms include intense throbbing pain, swelling of the gums and face, sensitivity to pressure when biting, fever, and a foul taste in the mouth from draining pus.
An untreated dental abscess can have serious health consequences, including the spread of infection to other parts of the head, neck, or even throughout the body via the bloodstream.
Chronic Infection
Some dead teeth develop chronic, low-grade infections that produce minimal symptoms or intermittent discomfort. These asymptomatic infections can persist for months or years, slowly destroying the bone around the tooth root. Even without obvious pain, these infections can compromise your overall health and weaken your immune system.
Factors Affecting the Timeline
Several variables influence how long tooth pain lasts before the nerve dies:
Extent of damage: A small cavity progresses more slowly than extensive decay or severe trauma. Cracks and fractures can accelerate nerve death by providing direct pathways for bacteria.
Individual immune response: People with stronger immune systems may experience prolonged inflammation as their bodies fight the infection, while those with compromised immunity might have faster nerve death.
Tooth location: Front teeth have single roots and may experience faster nerve death than multi-rooted molars with complex canal systems.
Blood supply: Teeth with robust blood flow may maintain nerve vitality longer, while those with compromised circulation deteriorate more rapidly.
Bacterial load: The type and virulence of bacteria involved affect the progression rate of infection and subsequent nerve death.
Warning Signs You Shouldn’t Ignore
Certain symptoms indicate your tooth nerve is in serious trouble and requires immediate dental attention. Persistent or worsening pain that doesn’t respond to pain relievers, prolonged sensitivity to hot or cold lasting more than 30 seconds, spontaneous pain without any trigger, visible discoloration of the tooth turning gray or dark, swelling in the gums or face, and the presence of a pimple-like bump on the gums near the painful tooth all warrant urgent evaluation.
Delaying treatment when these symptoms appear increases the risk of complications and may reduce the chances of saving the tooth.
Treatment Options for Dying Tooth Nerves
Modern dentistry offers effective solutions for saving teeth with dying nerves, allowing you to preserve your natural smile and prevent further oral health problems.
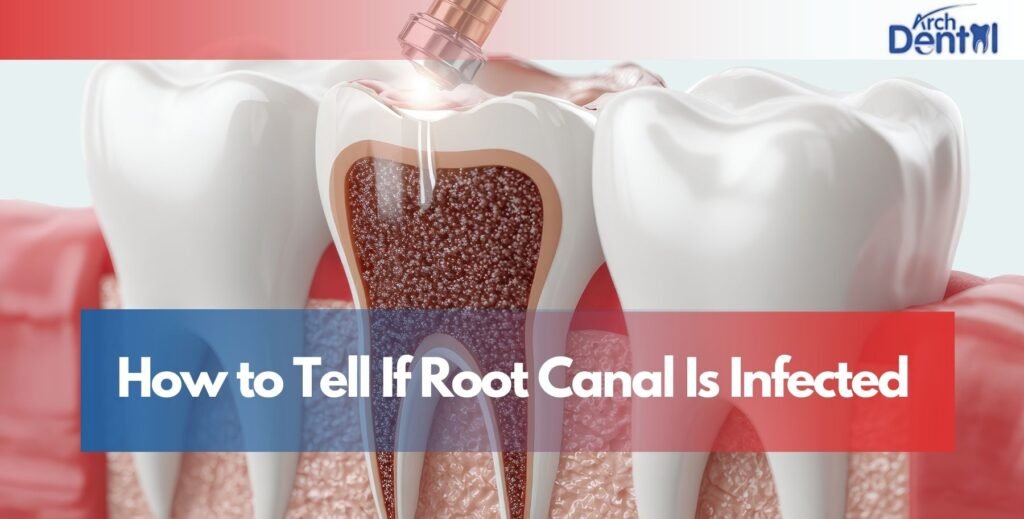
Root Canal Therapy
A root canal procedure remains the gold standard for treating a dying or dead tooth nerve. During this treatment, the dentist removes the infected or damaged pulp tissue, cleans and disinfects the root canal system, and seals it with filling material. This procedure eliminates infection, relieves pain, and allows you to keep your natural tooth.
Modern root canal techniques are much more comfortable than their reputation suggests, with most patients reporting minimal discomfort during and after the procedure.
Tooth Extraction
In cases where the tooth is too damaged to save, extraction may be necessary. While this immediately resolves the infection and pain, it creates the need for tooth replacement options like dental implants, bridges, or dentures to maintain proper oral function and aesthetics.
Conclusion
The duration of tooth pain before a nerve dies is unpredictable and varies widely among individuals, but typically spans from days to several months. However, the critical takeaway is that you should never wait for a tooth nerve to die on its own. The temporary relief you might experience after nerve death is misleading, as serious infection and complications often follow.
Early intervention offers the best outcomes, potentially saving your tooth and preventing the spread of infection. If you’re experiencing persistent tooth pain, don’t delay seeking professional care. A qualified Dentist in Northampton, MA can accurately diagnose the condition of your tooth’s nerve and recommend appropriate treatment to preserve your oral health and relieve your discomfort.
Remember, dental problems rarely resolve on their own and typically worsen without professional treatment. Protecting your smile means addressing tooth pain promptly rather than hoping it will simply go away.
Frequently Asked Questions
Can a tooth nerve heal itself without treatment?
In very early stages of inflammation (reversible pulpitis), a tooth nerve may heal if the irritant is removed through dental treatment like filling a cavity. However, once the damage progresses to irreversible pulpitis, the nerve cannot heal on its own and will eventually die without intervention.
Will the pain completely stop once the tooth nerve dies?
Many people experience temporary pain relief when the nerve dies, but this doesn’t mean the problem is solved. Pain typically returns when infection spreads beyond the tooth into surrounding tissues, often more severely than before.
How can I tell the difference between a dying nerve and other types of tooth pain?
Dying nerve pain is typically intense, persistent, and spontaneous, often described as throbbing or pulsating. It worsens with hot stimuli and may keep you awake at night. Other tooth pain from sensitivity or gum issues is usually triggered by specific stimuli and subsides quickly.
Is it safe to take antibiotics instead of getting dental treatment?
Antibiotics can temporarily reduce infection and pain, but they cannot eliminate the source of infection inside the tooth or save a dying nerve. Dental treatment is necessary to fully resolve the problem and prevent recurrence.
How long can I wait before getting treatment for tooth nerve pain?
You should seek dental care as soon as possible when experiencing persistent tooth pain. Waiting allows the condition to worsen, reduces treatment options, increases the risk of complications, and may ultimately result in tooth loss. Early treatment typically offers better outcomes and less invasive procedures.