Understanding which dental conditions necessitate restorative dental treatment helps you recognize when professional intervention is essential for preserving your oral health. Restorative dentistry encompasses procedures designed to repair damaged teeth, replace missing teeth, and restore full function to your smile. From simple cavities to complex reconstructions, various dental problems require restorative solutions that go beyond routine cleanings and preventive care. Recognizing the signs that indicate you need restorative work allows you to seek timely treatment, preventing minor issues from escalating into more serious complications. This comprehensive guide explores the specific conditions that demand restorative intervention, explaining how each problem affects your oral health and what treatment options can restore your smile to optimal condition.
Tooth Decay and Cavities Requiring Fillings
Tooth decay remains the most prevalent dental condition worldwide, affecting people of all ages and requiring restorative intervention to prevent progression and preserve tooth structure.
How Cavities Develop and Progress
Dental cavities form when bacteria in your mouth produce acids that dissolve tooth enamel, creating holes in the tooth structure. The process begins with plaque, a sticky film of bacteria accumulating on tooth surfaces, particularly in grooves, between teeth, and along the gum line. When you consume sugary or starchy foods, bacteria metabolize these carbohydrates and produce acids as byproducts. These acids attack enamel, causing demineralization that initially appears as white spots. Without intervention, the decay penetrates deeper, progressing through enamel into the softer dentin layer beneath. Once decay reaches dentin, it spreads more rapidly since this layer is less dense than enamel. Untreated cavities eventually reach the tooth pulp containing nerves and blood vessels, causing pain and potentially requiring root canal treatment instead of a simple filling.
Signs You Need a Filling
Recognizing symptoms indicating you have tooth decay prompts timely treatment before cavities expand and require more extensive restoration. Early cavities may produce no symptoms, which is why regular dental checkups are critical for detection. As decay progresses, you might experience sensitivity to sweet, hot, or cold foods and beverages. Visible signs include dark spots or holes in teeth, rough edges you can feel with your tongue, or food consistently getting stuck in the same location. Toothache ranging from mild discomfort to severe pain indicates significant decay requiring immediate attention. You might notice bad breath or an unpleasant taste despite good oral hygiene. Pain when biting down suggests deep decay near the tooth nerve. Any of these symptoms warrants scheduling a dental appointment promptly to prevent further damage.
Types of Filling Materials Available
Modern dental fillings come in various materials, each with specific advantages for different situations and patient preferences. Composite resin fillings are tooth-colored materials that bond directly to tooth structure, making them ideal for visible areas and small to medium cavities. They require less tooth removal than older materials and blend seamlessly with natural teeth. Amalgam fillings made from metal alloys offer exceptional durability for large cavities in back teeth that endure heavy chewing forces, though their silver color makes them less aesthetically pleasing. Porcelain or ceramic inlays and onlays provide superior aesthetics and durability for larger restorations but cost more than direct fillings. Gold fillings, though rarely used today, offer unmatched longevity. Your dentist recommends the best material based on cavity location, size, your bite forces, aesthetic concerns, and budget.
The Filling Placement Process
Getting a tooth filled is a straightforward procedure typically completed in one appointment lasting 30-60 minutes depending on cavity size and number. Your dentist numbs the area with local anesthesia ensuring you feel no pain during treatment. Using a dental drill or laser, they remove all decayed tooth structure, creating a clean cavity preparation. The space is disinfected and dried thoroughly. For composite fillings, a bonding agent is applied before placing the filling material in layers, with each layer hardened using a special light. The filling is then shaped to match your tooth’s natural contours and your bite is checked to ensure proper contact with opposing teeth. Final polishing creates a smooth surface. With proper care, fillings last 5-15 years depending on material and location.
Preventing Future Cavities
After receiving dental fillings, preventing new cavities protects your investment and preserves remaining natural tooth structure. Brush twice daily with fluoride toothpaste, spending at least two minutes covering all tooth surfaces. Floss daily to clean between teeth where cavities frequently develop and brushes cannot reach. Limit sugary and acidic foods and beverages that fuel bacteria and erode enamel. Drink water throughout the day to wash away food particles and maintain saliva flow that naturally protects teeth. Consider dental sealants for back teeth with deep grooves vulnerable to decay. Use fluoride mouth rinse for extra protection. Regular dental checkups every six months allow early detection of new cavities when they’re small and easily treated. These preventive measures dramatically reduce your risk of developing additional tooth decay requiring restorative treatment.
Broken, Cracked, or Fractured Teeth
Tooth fractures ranging from minor chips to severe breaks compromise tooth integrity and function, requiring restorative treatment to prevent further damage and restore appearance.
Common Causes of Tooth Damage
Teeth break for numerous reasons, with some fractures occurring suddenly while others develop gradually over time. Dental trauma from accidents, falls, or sports injuries causes immediate fractures that may be obvious or hidden within the tooth. Biting down on hard objects like ice, hard candy, popcorn kernels, or bones creates sudden force that cracks teeth. Using teeth as tools to open packages or crack nuts places excessive stress on tooth structure. Teeth grinding (bruxism) during sleep generates hundreds of pounds of pressure that wears down enamel and eventually causes cracks. Large dental fillings weaken remaining tooth structure, making these teeth more susceptible to fracture. Temperature extremes like drinking hot coffee followed immediately by ice water create expansion and contraction that can crack enamel. Age-related wear naturally weakens teeth over decades, increasing fracture risk.
Types of Tooth Fractures
Understanding the various tooth crack types helps explain why different restorative approaches are needed for each situation. Craze lines are superficial cracks in enamel that don’t cause pain and usually require no treatment beyond monitoring. Fractured cusps occur when a piece of the tooth’s chewing surface breaks off, typically around a filling, and usually don’t affect the tooth nerve. Cracked tooth syndrome involves a crack extending from the chewing surface toward the root, causing pain when chewing and temperature sensitivity. Split teeth result from untreated cracks that progress until the tooth separates into distinct segments, often requiring extraction. Vertical root fractures begin in the root and extend toward the chewing surface, frequently going unnoticed until infection develops. The fracture type determines whether the tooth can be saved and what restoration is appropriate.
Crowns for Extensively Damaged Teeth
Dental crowns provide the ideal solution for teeth with significant fractures, large fillings, or structural weakness that simple fillings cannot adequately restore. A crown completely covers the visible portion of the tooth above the gum line, protecting it from further damage while restoring shape, size, strength, and appearance. The procedure involves reshaping the damaged tooth to accommodate the crown, taking impressions or digital scans, and placing a temporary crown while the permanent restoration is fabricated. Modern porcelain crowns and zirconia crowns offer exceptional strength combined with natural appearance that matches surrounding teeth perfectly. Metal crowns provide maximum durability for back teeth where aesthetics matter less. Crown placement typically requires two appointments over 2-3 weeks, though same-day crowns are available with CAD/CAM technology. Crowns last 10-15 years or longer with proper care, allowing damaged teeth to function normally.
Bonding for Minor Chips and Cracks
Dental bonding offers a conservative, cost-effective solution for repairing minor chips, cracks, and cosmetic imperfections without removing significant tooth structure. The procedure involves applying tooth-colored composite resin directly to the damaged area, sculpting it to restore the tooth’s natural contour, and hardening it with a special light. Bonding can be completed in a single appointment lasting 30-60 minutes per tooth, usually without requiring anesthesia. The results blend seamlessly with your natural teeth, making repairs virtually invisible. While not as durable as crowns or veneers, bonding lasts 3-7 years with proper care and can be easily repaired if damaged. This treatment works beautifully for front teeth with minor chips, small cracks that don’t compromise tooth structure, or cosmetic reshaping to improve appearance. Bonding provides an affordable entry point to restorative dentistry for patients with budget constraints.
When Extraction Becomes Necessary
Severely fractured teeth with damage extending deep into the root or below the gum line may be impossible to restore, leaving extraction as the only viable option. Vertical root fractures, extensively split teeth, or fractures combined with severe decay often cannot be saved even with advanced techniques. Your dentist evaluates the fracture extent using x-rays and clinical examination, considering factors like remaining tooth structure, bone support, and overall prognosis. If extraction is recommended, discussing tooth replacement options immediately prevents complications from the empty space. Dental implants provide the most durable, natural-feeling replacement, though bridges and partial dentures offer alternatives. Leaving spaces where teeth were extracted allows neighboring teeth to shift, creates bite problems, and accelerates bone loss in the jaw. Prompt replacement maintains proper tooth alignment and jaw function.
Missing Teeth Requiring Replacement
Tooth loss creates functional problems and aesthetic concerns that restorative dentistry addresses through various replacement options restoring both appearance and chewing ability.
Consequences of Leaving Teeth Unreplaced
Failing to replace missing teeth triggers a cascade of problems affecting your remaining teeth, jawbone, facial structure, and overall health. Adjacent teeth drift into the empty space, becoming crooked and creating difficult-to-clean areas where decay and gum disease develop. Opposing teeth in the opposite jaw overerupt, losing proper contact and creating bite problems. Uneven chewing forces accelerate wear on remaining teeth. The jawbone in areas where teeth are missing begins resorbing (shrinking) since it lacks the stimulation from tooth roots, changing your facial appearance and making future tooth replacement more difficult. Missing back teeth force you to chew on one side, straining jaw joints and causing discomfort. Speech may be affected, particularly with front tooth loss. Self-consciousness about gaps in your smile impacts confidence and social interactions. Digestive issues can develop if missing teeth prevent proper food chewing.
Dental Implants as Permanent Solutions
Dental implants represent the gold standard for replacing missing teeth, providing permanent restorations that look, feel, and function like natural teeth. A titanium post is surgically placed into the jawbone where it fuses with the bone through osseointegration over 3-6 months. Once healed, a custom crown is attached to the implant, completing the restoration. Single tooth implants replace individual missing teeth without affecting adjacent healthy teeth. Multiple implants can support bridges or secure full dentures. Unlike other replacement options, implants preserve the jawbone by providing the stimulation bone needs to maintain density. They don’t require grinding down neighboring teeth like bridges do. Tooth implants last 20-30 years or longer with proper care, making them highly cost-effective despite higher initial investment. Implants restore full chewing power and confidence in your smile.
Fixed Bridges for Adjacent Missing Teeth
Dental bridges offer a non-surgical option for replacing one or more consecutive missing teeth by anchoring artificial teeth to adjacent natural teeth. Traditional bridges use crowns on teeth neighboring the gap to support the replacement tooth (pontic) suspended between them. The procedure requires reshaping adjacent teeth to accommodate crowns, taking impressions, and fabricating a custom bridge that’s permanently cemented in place. Fixed bridges restore chewing function and prevent tooth shifting while maintaining natural appearance. They typically last 10-15 years with proper care. Maryland bridges use a metal or porcelain framework bonded to the back of adjacent teeth, requiring minimal tooth preparation but offering less stability. While bridges provide good results, they depend on the health of supporting teeth and don’t prevent bone loss under the pontics like implants do.
Removable Partial Dentures
Partial dentures replace multiple missing teeth with a removable appliance that clips onto remaining natural teeth, offering an affordable tooth replacement solution. The denture consists of replacement teeth attached to a gum-colored plastic base, with metal or tooth-colored clasps that hook around natural teeth for retention. You remove the partial denture for cleaning and typically take it out at night. Modern partials are lighter, more comfortable, and more natural-looking than older versions. They restore basic chewing function and fill gaps in your smile, though they don’t feel as stable or natural as implants or bridges. Partial dentures require periodic adjustment as your mouth changes shape and typically need replacement every 5-8 years. They’re often used as temporary solutions while planning for more permanent restorations or when budget constraints prevent other options.
Complete Dentures for Full Tooth Loss
Full dentures replace all teeth in the upper or lower arch when extensive tooth loss has occurred, restoring basic function and facial appearance. Conventional dentures are made after remaining teeth are extracted and tissues have healed, usually 8-12 weeks post-extraction. Immediate dentures are placed the same day teeth are extracted, eliminating the period without teeth but requiring multiple adjustments as tissues heal and change shape. Complete dentures rest on your gums and rely on suction, muscle control, and adhesives for retention. They restore the ability to eat and speak, though with less efficiency than natural teeth. Modern dentures look remarkably natural, and dentists can customize appearance to match your facial features and age. Implant-retained dentures attach to 2-4 implants, providing dramatically improved stability and retention compared to traditional dentures while still being removable for cleaning.
Infected or Damaged Tooth Pulp
Tooth infections affecting the inner pulp tissue cause severe pain and can spread to surrounding structures, requiring immediate restorative treatment to save the tooth and prevent complications.
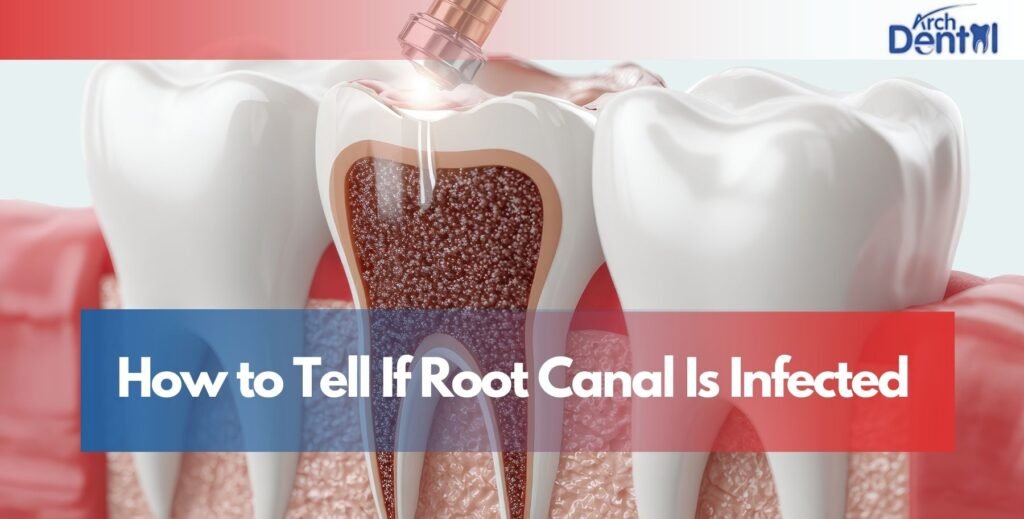
Understanding Root Canal Necessity
Root canal treatment becomes necessary when the pulp tissue inside a tooth becomes inflamed or infected, a condition that won’t heal on its own and worsens without intervention. The pulp contains nerves, blood vessels, and connective tissue extending from the tooth crown down through root canals into the jawbone. Pulp damage occurs from deep decay reaching the pulp chamber, cracks or chips exposing the pulp, repeated dental procedures traumatizing the tooth, or trauma from accidents. Symptoms indicating pulp problems include severe toothache, prolonged sensitivity to hot or cold, darkening of the tooth, swelling and tenderness in nearby gums, or a pimple-like bump on gums near the affected tooth. Sometimes pulp dies with no symptoms, detected only through x-rays showing infection at the root tip. Without treatment, the infection spreads into surrounding bone, potentially causing abscesses, facial swelling, bone loss, and systemic health problems.
The Root Canal Procedure Explained
Modern root canal therapy is comfortable and predictable, relieving pain rather than causing it as outdated reputation suggests. The procedure begins with local anesthesia numbing the tooth and surrounding area completely. Your dentist or endodontist creates an opening in the tooth crown, accessing the pulp chamber and root canals. Tiny instruments remove infected or damaged pulp tissue, and the canals are cleaned, shaped, and disinfected thoroughly. The empty canals are filled with a rubber-like material called gutta-percha and sealed to prevent reinfection. A temporary filling closes the access opening. Root canal treatment typically requires 1-2 appointments depending on infection severity and tooth location. Following treatment, the tooth needs a crown to protect it from fracture since removing the pulp makes teeth more brittle. The procedure has a 95% success rate, allowing treated teeth to function normally for many years.
Apicoectomy for Persistent Infections
When root canal treatment fails to resolve infection or cannot be performed due to tooth anatomy, an apicoectomy (root-end surgery) provides an alternative approach to saving the tooth. This surgical procedure involves accessing the infected area through the gum and bone, removing the tip of the tooth root and any infected tissue, then sealing the root end with a filling. Endodontic surgery is performed under local anesthesia with or without sedation for patient comfort. Recovery takes several days, with mild discomfort managed with pain medication. Success rates exceed 90%, making apicoectomy an effective solution when conventional root canal treatment is insufficient. The procedure allows tooth preservation that would otherwise require extraction, maintaining your natural tooth structure and preventing the need for replacement options.
Pulpotomy for Primary Teeth
Pulpotomy represents the pediatric equivalent of root canal treatment, used when decay or trauma affects the pulp of baby teeth (primary teeth). Since primary teeth naturally exfoliate, the procedure is simpler than adult root canals, removing only the infected pulp in the crown portion while leaving healthy pulp in the roots. The tooth is then restored with a filling or crown. This treatment preserves the primary tooth until it naturally falls out, maintaining proper spacing for permanent teeth and allowing normal chewing and speech development. Losing primary teeth prematurely can cause permanent teeth to erupt improperly, potentially requiring orthodontic treatment. Pulpotomy provides a conservative approach that saves primary teeth and prevents complications affecting permanent tooth development.
Post-Treatment Restoration Requirements
After completing root canal therapy, the tooth requires permanent restoration to protect it from fracture and restore full function. A dental crown is the standard restoration for back teeth (molars and premolars) that endure heavy chewing forces, as these teeth are particularly vulnerable to splitting after root canal treatment. Front teeth (incisors and canines) may be restored with crowns or large fillings depending on remaining tooth structure. The restoration is typically placed 1-2 weeks after root canal completion, once you’re symptom-free. Delaying permanent restoration risks tooth fracture that may make the tooth unrestorable. With proper restoration and care, root canal-treated teeth last as long as natural teeth often a lifetime. Regular dental checkups monitor the treated tooth’s health and catch any problems early.
Severe Wear and Erosion Needing Restoration
Tooth wear from various causes gradually destroys enamel and underlying tooth structure, eventually requiring restorative treatment to prevent further damage and restore proper function.
Causes of Excessive Tooth Wear
Multiple factors contribute to tooth enamel erosion and mechanical wear that compromise tooth integrity over time. Teeth grinding (bruxism) and jaw clenching, often occurring unconsciously during sleep, wear down tooth surfaces through constant friction and pressure. Acidic foods and beverages, citrus fruits, soda, sports drinks, wine—dissolve enamel through chemical erosion. Acid reflux and eating disorders like bulimia bathe teeth in stomach acid, causing rapid enamel loss. Aggressive brushing with hard-bristled toothbrushes abrades enamel, particularly near the gum line. Certain medications cause dry mouth, reducing saliva’s protective effects and increasing erosion risk. Occupational exposure to acids or airborne particles accelerates wear. Age naturally wears teeth over decades. These factors often combine, compounding damage and necessitating restorative intervention to preserve tooth structure and function.
Signs Your Teeth Need Restoration
Recognizing symptoms of dental wear prompts evaluation and treatment before damage becomes severe. Sensitivity to hot, cold, sweet, or acidic foods and beverages indicates enamel loss exposing dentin. Teeth appearing shorter or having flattened biting edges show significant wear. A yellower appearance develops as thin enamel reveals the yellow dentin underneath. Rough or irregular tooth surfaces feel different to your tongue. Chips or cracks appear along worn edges. Changes in bite or difficulty chewing suggest uneven wear affecting tooth alignment. Jaw pain or headaches may accompany teeth grinding. Cupping or grooves on chewing surfaces indicate erosion. These signs warrant dental evaluation to assess damage extent and discuss restoration options preventing further deterioration.
Full Mouth Reconstruction for Extensive Damage
Full mouth reconstruction addresses severe wear, erosion, or damage affecting multiple teeth throughout your mouth, comprehensively restoring function and aesthetics. This complex treatment involves coordinating multiple procedures: crowns, veneers, inlays, onlays, implants to rebuild your entire dentition. Treatment planning considers your bite alignment, jaw joint function, facial aesthetics, and oral health status. The process typically occurs in phases over several months, allowing healing between procedures. Temporary restorations maintain function and appearance during treatment. Comprehensive dental restoration dramatically improves your ability to chew, eliminates pain from worn teeth, and creates an aesthetically pleasing smile. While the investment is substantial, the functional and quality-of-life improvements are profound. Patients with severe wear often find reconstruction life-changing, restoring confidence and comfort they’d lost over years of progressive tooth damage.
Nightguards to Prevent Further Damage
Once teeth are restored, protecting them from continued grinding damage is essential for preserving your investment. Custom nightguards fabricated by your dentist provide superior protection compared to over-the-counter options. These appliances fit precisely over your teeth, distributing biting forces evenly and preventing direct tooth-to-tooth contact during grinding. Hard acrylic nightguards offer maximum durability for severe grinders, while softer versions provide comfort for mild cases. Wearing your nightguard consistently every night protects both natural teeth and restorations from excessive forces. Regular dental checkups monitor nightguard wear when it shows significant damage, it’s protecting your teeth as intended and may need replacement. Nightguards typically last 1-5 years depending on grinding severity. This simple preventive measure dramatically extends the lifespan of dental restorations and natural teeth.
Dietary Modifications to Reduce Erosion
Changing dietary habits significantly reduces acid erosion and protects restored teeth from further damage. Limit consumption of acidic beverages like soda, sports drinks, energy drinks, and fruit juices. When consuming acidic foods or drinks, finish them quickly rather than sipping over extended periods. Rinse your mouth with water afterward to neutralize acids. Wait 30-60 minutes before brushing after consuming acidic substances, as brushing immediately can damage acid-softened enamel. Use a straw when drinking acidic beverages to minimize contact with teeth. Choose water as your primary beverage throughout the day. If you have acid reflux, work with your physician to manage the condition effectively. These dietary adjustments protect both natural tooth structure and restorations, preventing the need for additional treatment in the future.
Conclusion
Numerous dental conditions necessitate restorative dental treatment, from common cavities and broken teeth to complex issues like infected pulp and severe wear. Recognizing the signs that indicate you need restorative care pain, sensitivity, visible damage, functional problems empowers you to seek timely treatment before minor issues become major complications. Modern restorative dentistry offers effective solutions for virtually any dental problem, with treatments ranging from simple fillings to comprehensive full mouth reconstruction. The key to successful outcomes lies in early intervention, following your dentist’s treatment recommendations, and committing to preventive care that protects your restored teeth. Whether you need a single filling or extensive restoration, today’s dental treatments can preserve your natural teeth and restore your smile to optimal health and beauty.
If you’re experiencing any dental problems or symptoms suggesting you need restorative dental treatment, consulting with a skilled dentist in Northampton, MA ensures you receive accurate diagnosis and comprehensive care. Professional evaluation identifies the specific condition affecting your teeth and creates a personalized treatment plan restoring your oral health and smile confidence.
Frequently Asked Questions
Who needs restorative dentistry?
Anyone with damaged, decayed, or missing teeth needs restorative dentistry. This includes people with cavities, broken teeth, tooth loss, worn enamel, infected tooth pulp, or failed previous dental work. Restorative treatments repair damage, replace missing teeth, and restore proper function and appearance to your smile.
What counts as restorative dental treatment?
Restorative dental treatment includes any procedure that repairs or replaces damaged or missing tooth structure. This encompasses fillings, crowns, bridges, dentures, dental implants, root canals, inlays, onlays, and full mouth reconstruction. These treatments restore teeth to normal function, prevent further damage, and improve smile aesthetics.
What is the most common type of dental restoration?
Dental fillings are the most common restoration, used to repair teeth damaged by cavities. Millions of fillings are placed annually to treat tooth decay. Composite (tooth-colored) fillings have become most popular due to their natural appearance and ability to bond directly to tooth structure.
What is restorative treatment for teeth?
Restorative treatment repairs damaged teeth or replaces missing teeth to restore normal oral function and appearance. It addresses problems caused by decay, fractures, wear, infection, or tooth loss. Treatments range from simple fillings to complex procedures like implants and full mouth reconstruction, all designed to preserve and restore dental health.
What is major restorative dental treatment?
Major restorative treatment includes complex, extensive procedures like crowns, bridges, dentures, dental implants, root canals, and full mouth reconstruction. These treatments typically cost more, require multiple appointments, and address severe damage or extensive tooth loss. Insurance often covers 50% of major restorative procedures after deductibles are met.